Dr Ben Wild
Overview |
The anterior chamber of the eye refers to the space between the cornea (the front clear tissue of the eye) and the iris (the colored part of the eye) where the aqueous humor (the liquid inside the eye resides). This area should be large, and clear of any debris.
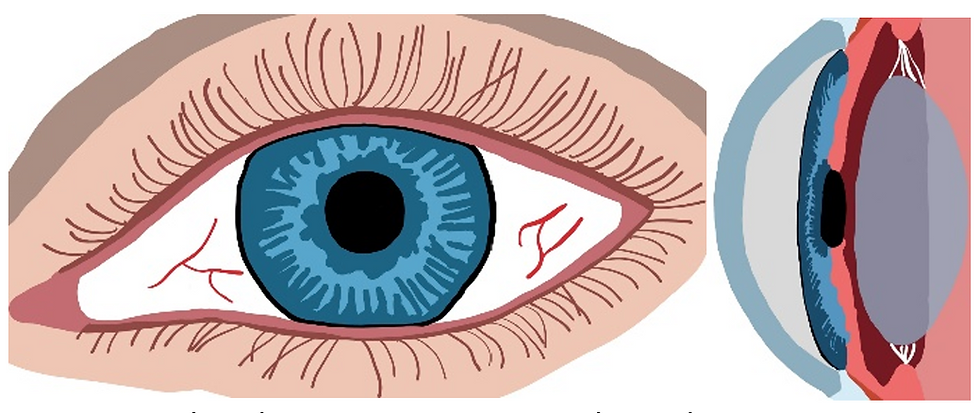
Front view (left) and sagittal view (right) of a healthy eye. The anterior chamber extends from the front of the lens to the back of the cornea.
Anterior uveitis, or iritis, refers to a condition where inflammation localized to the back of the iris (uveal layer) causes fibers and/or white blood cells to leak into the eye. Anterior uveitis can be classified as acute (usually develops quickly, in 1 eye and is the most symptomatic), recurrent (reoccurs after periods of no inflammation lasting over 3 months) or chronic (can present without symptoms, often occurs in both eyes and episodes last over 3 months). It can also be classified as granulomatous (produces clumps or nodules of immune cells) or non-granulomatous.
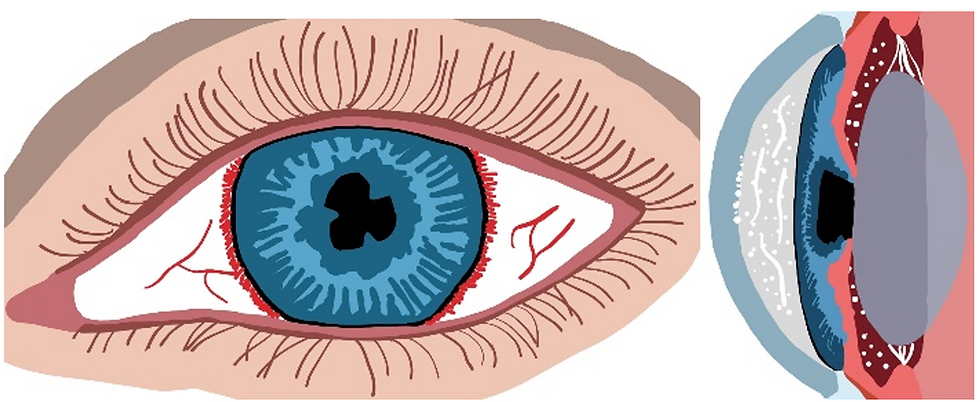
Front view (left) showing redness around the iris and synechiae (areas where the iris is stuck to the lens) and sagittal view (right) showing white blood cells, fibers and the iris stuck to the lens.
Signs and Symptoms |
Signs
Acute anterior uveitis | Redness around the iris, smaller pupil, white blood cells floating in the eye, white blood cells stuck to the inside of the cornea or to the iris, fibers floating around the anterior chamber, lower eye pressures, iris stuck to the lens of the eye. |
Chronic anterior uveitis | Change in color of the iris, clumps of white blood cells on the cornea or the iris, white blood cells floating in the eye, fibers floating around the anterior chamber, higher eye pressures, iris stuck to the lens of the eye, blood vessels growing on the iris, cataract, calcium depositing in the cornea, swelling of the macula (central retina). |
Symptoms
Acute anterior uveitis | Rapid onset, usually unilaterally, of pain, light sensitivity, redness, watery eyes, and blurriness if severe. |
Chronic anterior uveitis | Slowly progressing condition, sometimes asymptomatic, sometimes mild light sensitivity and/or pain. |
Causes and Risk Factors |
Causes
Infections (bacterial, viral, fungal, parasites), auto-immune conditions (rheumatoid arthritis, sarcoidosis, spondyloarthropathies, and many more), cancers, idiopathic (unknown).
Risk Factors
Ocular inflammation like dryness, conjunctivitis, etc.
Prevention, Investigation and Treatment |
Prevention
There are no known preventative measures.
Investigation
· If an episode is the 1st time, in one eye, non-granulomatous, and mild to moderate in severity then no investigation required.
· Otherwise, test for spondyloarthropathies, syphilis, sarcoidosis, Lyme disease, polyangiitis with granulomatosis, TB, and rheumatoid arthritis.
Treatments
· Steroid drops or ointments.
· Cyclogyl dilating drops.
· Steroid injections.
· Steroid pills.
· Non-steroidal anti-inflammatory pills.
· Disease modifying anti-rheumatic drugs.
Prognosis |
Prognoses vary wildly depending on what type of anterior uveitis is found. In most cases, early treatment can prevent any possible effects on vision long-term. If the uveitis is recurrent or chronic in nature, if it is due to an auto-immune condition, or if it is due to an infection, even with proper treatment, can lead to cataract formation, opacifying cornea, swelling of the retina (macula) or even permanent vision loss. The chances of these outcomes dramatically declines with routine eye examinations and proper treatment.
