Dr Ben Wild
Overview |
The cornea is the outermost layer of the eye in front of the colored iris. It is a clear tissue, void of any blood vessels, and is one of the main optical components responsible focusing light on the retina for proper vision. There are 5 layers within the cornea. The outermost layer is the epithelium responsible for creating a barrier against pathogens and foreign materials. This layer is attached to Bowman’s membrane which acts as a scaffold that connect the epithelium to the stroma. The stroma is the largest layer and is responsible for the cornea's rigidity and optical power. Descemet’s membrane is another scaffolding layer responsible for connecting the stroma to the endothelium. The endothelial layer is 1 cell thick and is responsible for pumping fluid out of the cornea so that the cornea doesn’t swell. Corneal dystrophies represent a collection of disorders that are categorized by the layer of the cornea they affect.



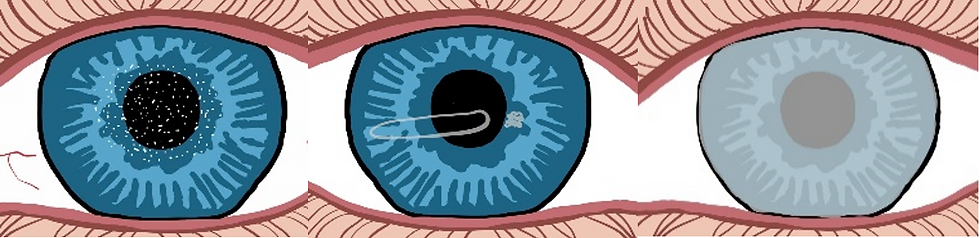
From left to right: top line (healthy eye, EBMD, Meesman), 2nd line (Reiss-Bucklers, Thiel Behnke, Lattice), 3rd line (Granular, Macular, Schnyder’s), 4th line (Fuch’s, Posterior polymorphous, Congenital hereditary endothelial).
Epithelial basement membrane dystrophy (EBMD) and Meesman dystrophy are the two main disorders that affect the corneal epithelium. EBMD is so common it has its own information page. Reiss-Bucklers (RB) and Thiel-Behnke (TB) dystrophies affect Bownman’s layer and affect the ability of the epithelium to stick to the remaining cornea. Lattice, granular, macular and Schnyder dystrophies represent the most common stromal dystrophies. Fuch’s dystrophy, posterior polymorphous dystrophy (PPD) and congenital hereditary endothelial dystrophy (CHED) all affect the endothelial layer. Fuch’s dystrophy is so common it has its own information page.
Signs and Symptoms |
Note: recurrent corneal erosions (RCEs) refer to the corneal epithelium sticking to the eyelids while sleeping and tearing open upon awakening. Refer to RCE information page.
Meesman | |
Reiss-Bucklers | Honeycomb opacities in Bowman's membrane, curly fibers, severe RCEs starting in children. |
Thiel-Behnke | Honeycomb opacities in Bowman's membrane, curly fibers, severe RCEs starting in children. |
Lattice | Dots that later connect into filaments that spread as the condition progresses in the stroma, RCEs later in life, blurred vision. |
Granular | Progressive white deposits in the shape of breadcrumbs in the stroma, glare, light sensitivity, blurring, RCEs. |
Macular | Progressive white dots that may be elevated in the stroma, RCEs, blur in 1st decade of life, haze. |
Schyder’s | Fluffy white opacities and crystals of fat and cholesterol in the stroma, blurring, glare, haze. |
Guttatta on the endothelium, folds in the cornea, swollen cornea, blurred vision for hours after awakening, pain. | |
Posterior polymorphous | Tiny bubbles or band like lesions on the corneal endothelium |
Congenital hereditary endothelial | Cloudy cornea, light sensitivity, watery eyes, blurred vision in newborns. |
Causes and Risk Factors |
Causes
Genetics.
Risk factors
Physical trauma (EBMD), irregular cholesterol or fat metabolism (Schnyder’s).
Prevention and Treatment |
Prevention
There are no known preventative measures.
Treatments
· Corneal transplant if vision is adversely affected by a stromal or endothelial dystrophy.
· Phototherapeutic keratectomy for epithelial and Bowman’s layer dystrophies.
· Treat the corneal swelling (see Fuch’s dystrophy information page).
· Monitor for glaucoma (for PPD).
Prognosis |
In most cases, most corneal dystrophies are asymptomatic and do not affect vision. Treatment for RCEs almost always solves the symptoms. If vision is affected, a corneal transplant can help restore vision but the dystrophy can recur in lattice, macular and granular. Also, a corneal transplant does not fully correct vision and hard plastic contacts may be needed instead of glasses. CHED on the other hand, will leave affected newborns with a lifetime of poor vision.
